What are my birthing options?
You may be trying to decide what kind of birth you’d like, particularly between vaginal birth or C-section. If so, speak to your midwife or doctor as soon as possible. They can give you the information and support you need to understand the different types of birth and make the right choice for you.
On this page
Can I choose what type of birth I want?
Birth interventions and consent
Anxiety about labour and birth
Can I have a C-section if I don’t have a medical reason?
Can I get a second medical opinion on my birthing options?
Types of birth
Birth is different for everyone, and you will have choices to make about how it happens. The two most obvious birthing options are:
- Vaginal birth (when your baby comes through your vagina. This can be with or without extra help such as forceps or ventouse).
- Caesarean section, or C-section (when your baby is delivered through a cut in your tummy and womb).
You will have other choices to make, including:
- where to give birth, for example in a hospital, a birth centre or in your home
- pain relief options, whether to to have it, and if you do the kind of pain relief you have
- whether you would like to try a water birth.
Before or during labour you may have choices to make about whether to have an intervention (medical help with labour), such as induction of labour or assisted labour if the labour is not progressing or for another reason.
Read more about making decisions in pregnancy - risks, benefits, consent and your rights.
Can I choose what type of birth I want?
It’s helpful to consider these different birth options while you’re pregnant. Then you can decide what you’d like to aim for and tell any birth partners and your medical team.
Generally, you can choose how and where you give birth, unless you’re not well enough to give your choices and consent.
That said, you may change your mind during labour. Things can happen that cause a change of plan. Your midwife will support you through this.
As well as your choices, the type of birth you have will depend on your and your baby’s health and other things like your age and weight.
If are not able to give your consent, it can be the time when your birth partner can step in to tell your care team about the choices you’ve talked about.
If you have a birth partner, it’s also important that they know you may change your mind about what you want and support you in that.
Birth interventions and consent
You may have preferences about the interventions (medical help) that midwives and doctors can offer if they think you need help to safely deliver your baby. Interventions include:
- induction of labour (when a doctor or midwife brings on labour artificially)
- assisted vaginal delivery (when a cut is made in the area between your vagina and anus, or when a vacuum or forceps are used to guide your baby out)
- a c-section that was not planned.
They can offer these but it will be your decision. Doctors cannot give you treatment you do not want, unless you’re not able to give consent, for example in an emergency.
If there are labour interventions you would prefer not to have, it’s better to tell your midwife about this in advance so that you can talk with them about the risks and benefits ahead of time.
As well as this you can include them on your birth plan. Birth plans can help you to feel more reassured and in control ahead of giving birth.
Birthrights has more information about your rights during pregnancy and birth.
Anxiety about labour and birth
You may be worried or anxious about the pain of a vaginal birth, or you may have had a difficult vaginal birth before. You may also have had a pregnancy loss that is making you anxious about the safety of the baby. You can read more here about past experience of trauma and how it might affect your decisions.
Speak to your midwife if you’re feeling anxious or worried. They will support you and help you make choices that feel right for you.
You can talk though the birth and what you would prefer, including what you would and wouldn’t like to happen.
Knowing the risks and benefits of some choices beforehand will mean that you are in a good place to make a decision. For example you could read about induction of labour (starting your labour before it starts naturally) early on just in case this is an option for you to consider.
A severe fear of childbirth (called tokophobia) is something that trained health care professionals can support you with. Speak to your midwife about getting help.
Read more about tokophobia and possible treatments.
Past trauma
Your past experiences may affect how you choose to give birth. For example, if you have gone through sexual abuse.
Speak to your midwife, doctor, or a healthcare professional you trust about your concerns. It’s up to you how much you tell them about what has happened to you in the past.
They will help you plan what you would and would not like to happen during labour. For example, some survivors of sexual abuse may want to avoid internal vaginal examinations (where the midwife or doctor looks inside your vagina).
You need to give permission for all examinations to happen. If you plan to say no to these, include it in your birth plan and talk about it with your midwife as soon as you can.
Your midwife or doctor may refer you to a health professional who specialises in mental health for more support.
Can I have a C-section if I don’t have a medical reason?
If you ask for a c-section without a medical reason, your midwife or doctor will talk through the risks and benefits with you.
If after this, you still don’t want a vaginal birth, your doctor should offer you a planned c-section or refer you to another doctor who will do it.
Find out more about the benefits and risks of a c-section.
Choosing the type of birth you have may feel daunting. Although everyone’s different, it may be reassuring for you to know that most women in the UK recover well and have healthy babies whether they have a vaginal or c-section birth.
Can I get a second medical opinion on my birthing options?
You can ask your midwife to refer you to another health professional to speak about your birth with, such as:
- an obstetrician (a doctor who specialises in care during pregnancy, labour and after birth)
- an anaesthetist (a doctor who gives anaesthetic for medical operations and procedures)
- a senior or consultant midwife
- a mental health specialist.
Your healthcare team should do all they can to support you to have the birth that you want.
While this doesn’t happen for every woman and birthing person, a 2022 study found that midwives strongly want to support decisions made by the people in their care.
One example of this is Laura’s experience:
“‘I asked for a c-section because I had a difficult first birth followed by postnatal depression and post-traumatic stress. The team looking after me reassured me throughout my pregnancy but reminded me of my other birth options. They helped with my birth plan, which included different options, including a planned c section, trying a vaginal birth and what would happen if I went into labour early. Having this reassurance reduced my anxiety and helped me feel confident about what I wanted for the birth.”
Laura
The BRAIN acronym
Using the BRAIN (or BRAINS) acronym can be helpful when you’re making decisions about your care. Make a note of it and use it to help shape and communicate your birth preferences.
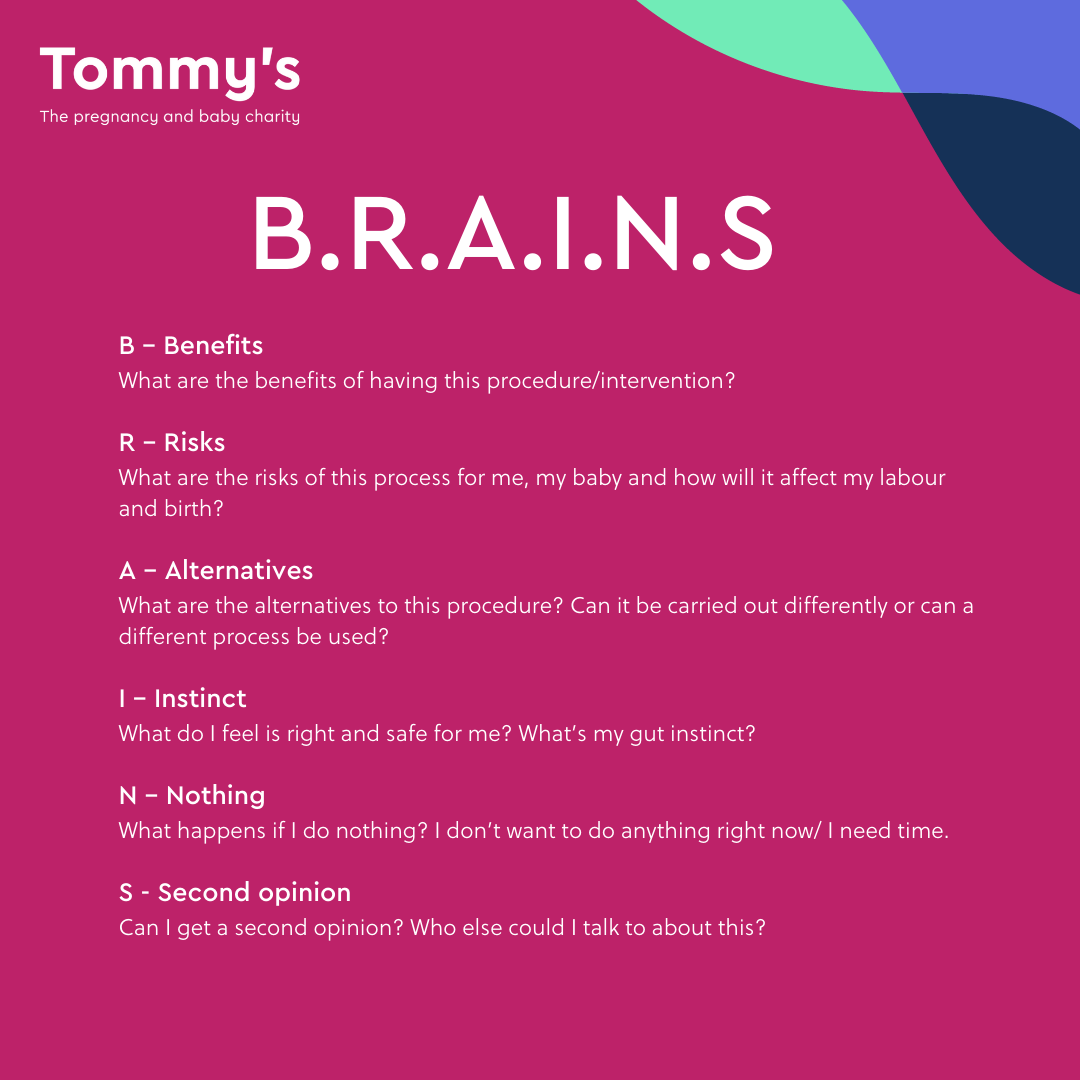
B - Benefits
What are the benefits of having this procedure/intervention?
R - Risks
What are the risks of this process for me, my baby and how will it affect my labour and birth?
A - Alternatives
What are the alternatives to this procedure? Can it be carried out differently or can a different process be used?
I - Instinct
What do you feel is right and safe for me? What's my gut instinct?
N - Nothing
What happens if I do nothing? I don’t want to do anything right now/ I need time.
Some health care sources and providers include an S which stands for:
Second opinion
Can I get a second opinion from another doctor/ midwife? Who else could I talk to about this? Friends, family or my partner?
Read more about making informed decisions in pregnancy.
Kloester, J., Willey, S., Hall, H. and Brand, G. (2022). Midwives’ Experiences of Facilitating Informed decision-making – a Narrative Literature Review. Midwifery, [online] 109(109), p.103322. doi: https://doi.org/10.1016/j.midw.2022.103322.
National Institute for Health and Care Excellence (2021). Overview | Caesarean birth | Guidance | NICE. [online] www.nice.org.uk. Available at: https://www.nice.org.uk/guidance/ng192 [Accessed 30 Aug. 2024].
National Institute for Health and Care Excellence (NICE) (2020). Antenatal and Postnatal Mental health: Clinical Management and Service Guidance | Guidance | NICE. [online] Nice.org.uk. Available at: https://www.nice.org.uk/guidance/cg192 [Accessed 30 Aug. 2024].
NICE (2022). Your care | Making decisions about your care | NICE and the public | NICE Communities | About. [online] NICE. Available at: https://www.nice.org.uk/about/nice-communities/nice-and-the-public/public-involvement/making-decisions-about-your-care/your-care [Accessed 30 Aug. 2024].
NICE (2023). Overview | Intrapartum care | Guidance | NICE. [online] www.nice.org.uk. Available at: https://www.nice.org.uk/guidance/ng235/ [Accessed 30 Aug. 2024].
RCOG (2019). Considering a caesarean birth | RCOG. [online] RCOG. Available at: https://www.rcog.org.uk/for-the-public/browse-our-patient-information/considering-a-caesarean-birth/ [Accessed 30 Aug. 2024].
Schei, B., Lukasse, M., Ryding, E.L., Campbell, J., Karro, H., Kristjansdottir, H., Laanpere, M., Schroll, A.-M., Tabor, A., Temmerman, M., Van Parys, A.-S., Wangel, A.-M. and Steingrimsdottir, T. (2014). A History of Abuse and Operative Delivery – Results from a European Multi-Country Cohort Study. PLoS ONE, [online] 9(1). doi: https://doi.org/10.1371/journal.pone.0087579.
The Survivors Trust (2019). Pregnancy, Birth and Parenthood after Childhood Sexual Abuse - The Survivors Trust. [online] thesurvivorstrust.org. Available at: https://thesurvivorstrust.org/research/pregnancy-birth-and-parenthood-after-childhood-sexual-abuse/ [Accessed 30 Aug. 2024].
Read blogs and stories about giving birth
-
Read more about ''Baby boxes' are trialed for the first time in the UK 'Giving birth blogs
'Baby boxes' are trialed for the first time in the UK
-
Read more about 'What we want to see on One Born Every Minute 'Giving birth blogs
What we want to see on One Born Every Minute
-
Read more about 'Jade’s water birth experience 'Giving birth blogs
Jade’s water birth experience
-
Read more about 'The UK opens first maternity clinic for victims of sexual assault and rape 'Giving birth blogs
The UK opens first maternity clinic for victims of sexual assault and rape

